When calling the surgical or gastro registrar on the phone, one of the surefire questions you will be asked is ‘is the patient hemodynamically stable?’ This is no doubt an important question but unfortunately hemodynamic stability means different things to different people. There is generally a lack of willingness to look beyond a ‘normal’ vs ‘low’ blood pressure.
It should be made clear that hypotension is a sign of ‘decompensated’ shock. The idea that hypotension is a late sign of shock has been long recognized in the trauma literature where 18% of penetrating abdominal trauma can have over 750ml of blood in the abdomen despite normal vital signs (including 7% who had over 1500ml). In the majority of patients evidence of tissue hypoperfusion precedes the development of hypotension (1).
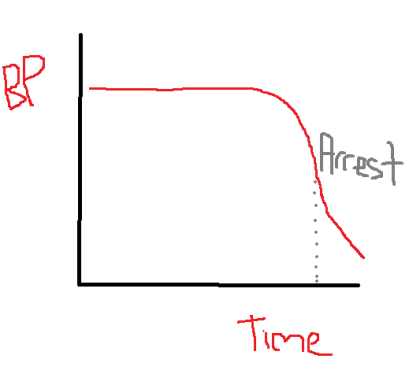
Why is this? Well, it is all about the concept that pressure does not equal flow. The body is quite adept at trying to maintain a normal blood pressure through various compensatory mechanism, chief amongst which is the sympathetic response. But this does not tell us whether perfusion at the tissue level is adequate- inadequacy of this is after all the definition of shock. This is especially true in young patients where the compensatory mechanisms are quite strong and blood pressure may be preserved till late in the piece, as illustrated by the graph at the top, of my creation (credit to MS paint).
This phenomenon is true in all situations- not just trauma- so it is relevant to the patients you will be seeing on ward calls. For example ‘normotensive shock’ is recognized in sepsis (2), cardiogenic shock (3), and just generally (4). What then are the signs of ‘normotensive shock’ you should look out for? Well, these are simply the signs of inadequate tissue perfusion- cool and clammy skin, oliguria, mental state changes and elevated lactate. Other signs which may accompany this that are not necessarily indicative of hypoperfusion but that do indicate a compensatory response are tachycardia and tachypnea.
It is also important to note two slightly related things. Firstly, a systolic blood pressure of 110 may be normal for a 20 year old but grossly hypotensive for a 70 year old with chronic hypertension. Secondly, it is sometimes difficult to tell whether a ‘soft’ blood pressure in a young person is just normal for them or whether they are actually hypotensive- a normal heart rate cannot be used to reassure you in this instance because not uncommonly shocked patients may have paradoxically increased parasympathetic tone (1) the exact mechanism for which is unclear. Older patients may also be on Beta Blockers.
The conclusion in all of this- next time you call the gastro reg with a patient who has vomited blood and is clammy with a lactate of 4 but has a normal blood pressure, the answer to the question ‘is the patient hemodynamically stable?’ is a ‘HELL NAH”.
Today’s post may sound basic but it is all about fundamentals- a fundamental which is often simply not done. Rather than spending 10 minutes documenting dual heart sounds, look and feel for the signs of shock!
Till next time.
- Identification and Resuscitation of the Trauma Patient in Shock Michael N. Cocchi, MDa , Edward Kimlin, MDa , Mark Walsh, MDb , Michael W. Donnino, MD. Emerg Med Clin N Am 25 (2007) 623–642
- Septic Shock. Advances in Diagnosis and Treatment. Christopher W. Seymour, MD, MSc and Matthew R. Rosengart, MD, MPH. JAMA. 2015 Aug 18; 314(7): 708–717.
- Menon V et al. Acute myocardial infarction complicated by systemic hypoperfusion without hypotension: Report of the SHOCK trial registry. Am J Med 2000 Apr 1 108 374380
- Approach to Hemodynamic Shock and Vasopressors. Stefan Herget-Rosenthal, Fuat Saner and Lakhmir S. Chawla. CJASN March 2008, 3 (2) 546-553; DOI:https://doi.org/10.2215/CJN.01820407
You must be logged in to post a comment.