Today’s post regards a common pitfall regarding the assessment of the hypotensive patient. Unfortunately, it will be based on anecdote rather than literature, but hopefully you won’t find the underlying assumptions too controversial.
Often you are called to the bedside of a patient with a hypotensive episode. You arrive to find them flattened on the bed, sometimes in the Trendelenburg position. You take stock of the situation and find the airway to be intact, the patient fully responsive, with warm peripheries and a good strong peripheral pulse. They are breathing comfortably. A blood pressure is taken and this is 110/70. The other vitals are normal as is the rest of the examination.
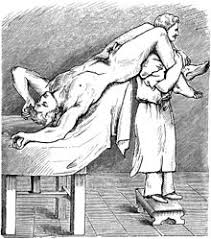
It is easy to conclude that the blood pressure has normalised and that this was therefore a self- resolving period of hypotension, most likely postural or vasovagal. What is important to remember is that, if you leave at this point, you have left the patient in a highly unnatural position. People don’t live their lives supine, nor indeed in Trendelenburg, and often their previous blood pressure recording taken in hospital will be with them sitting up. It is easy to gloss over this fact as you only arrive after the fact and therefore tend to only ever see the patient supine.
Before being reassured that the blood pressure is normal you must make sure it is normal in the sitting position. If they are sat up and now the blood pressure is 85/40, you clearly have an ongoing problem. Even the most posturally fragile old patients should maintain a normal blood pressure while sitting.
I have certainly ignored my own rule multiple times and it is extremely easy to do so because the human mind tends to only see what is there in front of you. Also, given the multitude of calls for abnormal vital signs, we latch onto any indication that the patient is actually OK and doesn’t need intervention. A few times when I ignored this rule I was later called for sustained hypotension (of course after they had been sat up) which turned out to be proper pathology.
The first of many lessons that you always need to take into account what we have done to the patient when making your assessment!